Solar Law knows how to respond when a child suffers brain injury. The firm has successfully prosecuted many cases involving injuries to the brain. Its success is the result of its knowledge, skill, and ability to assemble a team of highly accomplished experts.
The human brain is the most complex organ in the human body. If the Human brain is an orchestra, executive functioning and self-regulation are its conductor. This essential power derives from a set of skills that depends on three types of brain function: working memory, mental flexibility, and self-control. Children aren’t born with these skills—they are born with the potential to develop them. A healthy brain is essential for the acquisition of these functions.
Despite its remarkably protective skull, the fluid that cushions it, and the defensive barrier that isolates it from the bloodstream, the human brain is not invincible. It is subject to traumatic or acquired brain injury.
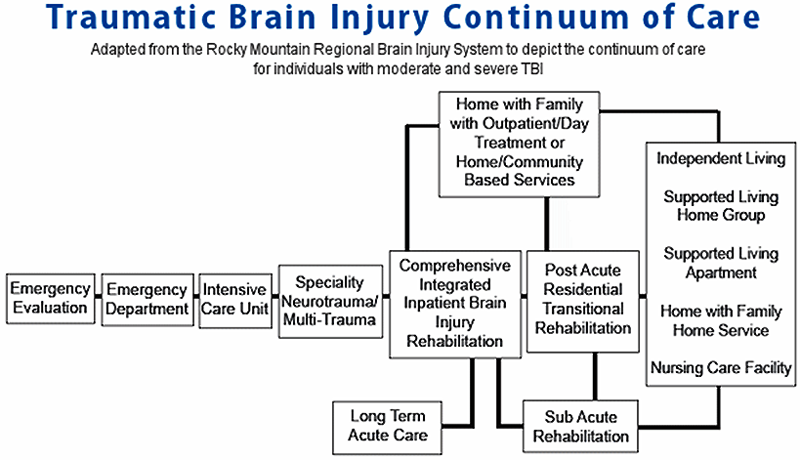
Just as no two people are exactly alike, no two brain injuries are exactly alike. For some, brain injury is the start of a lifelong disease process. The injury requires access to a full continuum of medically necessary treatment and community-based support furnished by interdisciplinary teams of qualified, specialized clinicians working in accredited programs and appropriate settings.
The individual who sustains a brain injury and his or her family are the most important members of the treatment team. Their choices, goals and cultural, religious, social and economic backgrounds must always be taken into consideration in treatment planning.
The Brain Injury Association of America endorses the Brain Trauma Foundation’s Guidelines for the Management of Severe Brain Injury and the Colorado Traumatic Brain Injury Medical Treatment Guidelines.
Treatment Continuum
The diagram below depicts brain injury treatment in an orderly progression from trauma care to community integration. But very little about brain injury is orderly. Individuals who sustain brain injuries may enter, exit and re-enter treatment at any point along the continuum. Treatment may be needed continuously or on an intermittent basis throughout the individual’s lifespan.
Facility and Program Types
Intensive Care Unit (ICU) After receiving emergency medical treatment, persons with a moderate to severe brain injury may be admitted to a hospital’s Inpatient Intensive Care Unit. The goals in the ICU include achieving medical stability, medical management, and prevention of medical crisis. Some preventive rehabilitation may be initiated in the Intensive Care Unit such as body positioning, splinting, and range of motion (a therapist moves the person’s limbs).
Persons treated in the ICU may be unconscious, in a coma, and medically unstable. Many tubes, wires, and pieces of medical equipment may be attached to the patient to provide life sustaining medical care. Medical equipment frequently used in the ICU includes:
A Ventilator (also called a Respirator) is a machine that helps a person breathe.
- A person who has sustained a brain injury may be unable to breathe on his or her own. To use a ventilator, a tube is placed through the person’s mouth to the breathing passage (trachea, “windpipe”). This procedure is called intubation.
Intubation with the use of a ventilator allows a person to breathe and receive oxygen, which is necessary for life. - Intravenous lines (IVs) are tubes placed in a person’s veins to deliver medications and fluids to the person’s body.
- Arterial lines are tubes placed in a person’s arteries to measure blood pressure.
- A Foley Catheter is used to collect and monitor a person’s urine output.
- A person who has sustained a brain injury may be unable to control bladder functions.
- A rubber tube is inserted into the person’s bladder. This allows urine to move from the bladder, through the tube, and to a container at the end of the tube.
- A Nasogastric Tube (NG Tube) is used to deliver medication and nutrients directly to a person’s stomach.
- A person who has sustained a brain injury may be unable to swallow.
- A tube is placed through a person’s nose or mouth and run through the swallowing passage (the esophagus), to the stomach.
- An EKG machine monitors a person’s heart.
- Wires with sticky ends are placed on the body.
- An Intracranial Pressure (ICP) Monitor is a device attached to a person’s head with a monitor that indicates the amount of pressure in the brain.
- When the brain is injured it may swell.
- When the brain swells, the brain has no place to expand. This can cause an increase in intracranial pressure (the pressure within the skull).
- If the brain swells and has no place to expand, this can cause brain tissues to compress, causing further injury.
- A Pulse Oximeter is a small, clamp-like device placed on a person’s finger, toe or earlobe. The Pulse oximeter measures the amount of oxygen in the blood stream.
Acute Rehabilitation
As early as possible in the recovery process, individuals who sustain brain injuries will begin acute rehabilitation. The treatment is provided in a special unit of the trauma hospital, a rehabilitation hospital or another inpatient setting. During acute rehabilitation, a team of health professionals with experience and training in brain injury work with the patient to regain as many activities of daily living as possible. Activities of daily living include dressing, eating, toileting, walking, speaking, and more.
Post acute Rehabilitation
When patients are well enough to participate in more intensive therapy, they may be transferred to a post acute rehabilitation setting such as a residential rehabilitation facility. The goal of post-acute rehabilitation is to help the patient regain the most independent level of functioning possible. Rehabilitation channels the body’s natural healing abilities and the brain’s relearning processes so an individual may recover as quickly and efficiently as possible. Rehabilitation also involves learning new ways to compensate for abilities that have permanently changed due to brain injury. There is much that is still unknown about the brain and about brain injury rehabilitation. Treatment methods and technologies are rapidly advancing as knowledge of the brain and its function increases.
Subacute Rehabilitation
Patients who cannot tolerate intensive therapy may be transferred to a subacute rehabilitation facility. Subacute rehabilitation programs are designed for persons with brain injury who need a less intensive level of rehabilitation services over a longer period. Subacute programs may also be designed for persons who have made progress in the acute rehabilitation setting and are still progressing but are not making rapid functional gains. Subacute rehabilitation may be provided in a variety of settings, often a skilled nursing facility or nursing home.
Day Treatment (Day Rehab or Day Hospital)
Day treatment provides rehabilitation in a structured group setting during the day and allows the person with a brain injury to return home at night.
Outpatient Therapy
Following acute, post-acute or subacute rehabilitation, a person with a brain injury may continue to receive outpatient therapies to maintain and/or enhance their recovery. Individuals whose injuries were not severe enough to require hospitalization or who were not diagnosed as having a brain injury when the incident occurred may attend outpatient therapies to address functional impairments.
Home Health Services
Some hospitals and rehabilitation companies provide rehabilitation therapies within the home for persons with brain injury.
Community Re-entry
Community re-entry programs generally focus on developing higher level motor, social, and cognitive skills to prepare the person with a brain injury to return to independent living and potentially to work. Treatment may focus on safety in the community, interacting with others, initiation and goal setting and money management skills. Vocational evaluation and training may also be a component of this type of program. Persons who participate in the program typically live at home.
Independent Living Programs
Independent living programs provide housing for persons with brain injury with the goal of regaining the ability to live as independently as possible. Usually, independent living programs will have several different levels to meet the needs of people requiring more assistance and therapies, as well as those who are living independently and being monitored.
Medications
Medications for persons with brain injury are carefully selected, prescribed, and monitored by the physician on an individual basis. The physician or pharmacist can explain a medication’s purpose, side effects and precautions to you. A general explanation of medication groups is described below.
- Analgesics may be used for pain relief and pain management.
- Anti-Anxiety Agents may lessen feelings of uncertainty, nervousness, and fear.
- Anti-Coagulants may be used to prevent blood clots.
- Anti-Convulsants may be used to prevent seizures.
- Anti-Depressants may be used to treat symptoms of depression.
- Anti-Psychotics may be used to target psychotic symptoms of combativeness, hostility, hallucinations, and sleep disorders.
- Muscle Relaxants may be used to reduce muscle spasms or spasticity.
- Sedative-Hypnotic Agents may be used to induce sleep or depress the central nervous system in areas of mental and physical response, awareness, sleep, and pain.
- Stimulants may be used to increase levels of alertness and attention.
Alternative Medicine and Brain Injury
Alternative medicines, including alternative therapies, are an under-researched area of brain injury treatment. The National Center for Complementary and Alternative Medicine (part of the National Institutes of Health) offers a Guide to Complementary and Alternative Medicines. The Brain Injury Association also published an issue of the Challenge! newsletter about alternative medicine and brain injury.
Healthcare Professionals
Physiatrist
is a doctor of physical medicine rehabilitation. The physiatrist typically serves as the leader for the rehabilitation treatment team and makes referrals to the various therapies and medical specialists as needed. The physiatrist works with the rehabilitation team, the patient, and the family to develop the best possible treatment plan.
Physical Therapists
evaluate and treat a person’s ability to move the body. The physical therapist focuses on improving physical function by addressing muscle strength, flexibility, endurance, balance, and coordination. Functional goals include increasing independent ability with walking, getting in and out of bed, on and off a toilet, or in and out of a bathtub. Physical therapists provide training with assistive devices such as canes or walkers for ambulation. Physical therapists can also use physical modalities, treatments of heat, cold, and water to assist with pain relief and muscle movement.
Occupational Therapists
use purposeful activities as a means of preventing, reducing, or overcoming physical and emotional challenges to ensure the highest level of independent functioning in meaningful daily living. Areas addressed by occupational therapists include: feeding; swallowing; grooming; bathing; dressing; toileting; mobilizing the body on and off the toilet, bed, chair, bathtub; thinking skills; vision; sensation; driving; homemaking; money management; fine motor (movement of small body muscles, such as in the hands); wheelchair positioning and mobility; home evaluation; durable medical equipment assessment and training (such as, use of a raised toilet seat to assist with getting on and off the toilet more easily). The occupational therapist also fabricates splints and casts to reduce deformities and optimize muscle functioning.
Speech/Language Pathologists
evaluate a person’s ability to express himself (speech, written, or otherwise expressed) as well as comprehend what is seen or heard. A speech/language pathologist trains a person to use assistive technology as an alternative form of communication if the person is unable to verbalize. The speech/language pathologist focuses on the muscles in the face, mouth, and throat. They also address swallowing issues.
Rehabilitation Nurses
monitor all body systems. A rehabilitation nurse attempts to maintain the person’s medical status, anticipate potential complications, and work on goals to restore a person’s functioning. A rehabilitation nurse is responsible for the assessment, implementation, and evaluation of each individual patient’s nursing care and educational needs based on specific problems as well as coordinating with physicians and other team members to move the patient from a dependent to an independent role.
Case Managers/Social Workers
are responsible for assuring appropriate and cost-effective treatment and the facilitation of discharge planning. Maintains regular contact with the patient’s insurance carrier, family, and referring physician to assure that treatment goals are understood and achieved.
Recreational Therapists
provide activities to improve and enhance self-esteem, social skills, motor skills, coordination, endurance, cognitive skills, and leisure skills. Recreational therapists plan community outings to allow the person to directly apply learned skills in the community. Additional programs provided by recreational therapists may include pet therapy, leisure education, wheelchair sports, gardening, special social functions or holiday functions for persons and their family.
Neuropsychologists
focus on thinking skills, behavior, and emotional processing. Neuropsychologists provide services to reduce the impact of setbacks and to help the person return to a full productive life. The neuropsychologist’s evaluations provide valuable information to assist with school, community, or employment re-entry.
Aquatic Therapists
are occupational therapists, physical therapists, or recreational therapists with specialized training to provide therapy in a heated water pool. Aquatic therapists assist a person to increase strength, coordination, ambulation skills, endurance, muscle movement, and reduce pain. The goal is to increase the person’s functional ability with activities of daily living.
Scales and Measurements of Functioning
Several scales and measures are used to rate and record the progress a person makes in rehabilitation following a brain injury. The most common ones are described below.
Disability Rating Scale (DRS)
The Disability Rating Scale (DRS) measures an individual’s general functional change over the course of recovery and rates an individual’s level of disability from None to Extreme. This scale considers cognitive and physical function, impairment, disability and handicap to present a global depiction of the individual’s disability. The DRS can track an individual’s progress from “coma to community.”
Functional Independent Measure (FIM)
The Functional Independent Measure (FIM) is a scale that rates an individual’s independence level with activities of daily living. Activities of daily living include self-care, bowel and bladder management, locomotion, transfers, communication, and social cognition. FIM scores range from 1-complete dependence to 7-complete independence.
Functional Assessment Measure (FAM)
The Functional Assessment Measure (FAM) is used in conjunction with the Functional Independent Measure (FIM). The FAM was developed specifically for people with brain injury and consists of 12 items added to the 18 items of the Functional Independence Measure (FIM).
Learn More about Brain Injuries
What is the difference between an acquired brain injury and a traumatic brain injury?
Traumatic brain injury (TBI)
A traumatic brain injury (TBI) is an injury to the brain caused by an external force after birth. Common causes of a traumatic brain injury include gunshot wounds, motor vehicle crashes, assaults, or falling and striking your head.
The Brain Injury Association further officially defines TBI “as an alteration in brain function, or other evidence of brain pathology, caused by an external force.”
Acquired brain injury (ABI)
An acquired brain injury (ABI) includes all types of traumatic brain injuries and brain injuries caused after birth by cerebral vascular accidents (commonly known as stroke), and loss of oxygen to the brain (hypoxic brain injury).
The Brain Injury Association’s official definition of ABI is “an injury to the brain, which is not hereditary, congenital, degenerative or induced by birth trauma. An acquired brain injury is an injury to the brain that has occurred after birth.”
Injuries to the brain that are present at birth or progressive in nature, such as Alzheimer’s disease or Parkinson’s, are not considered a traumatic or acquired brain injury.
Cerebral Palsy
is a broad term referring to neurological disorders affecting body movement and muscle coordination. The cause varies from case to case and can include oxygen-depriving (hypoxic) injury to the brain, traumatic injury, infection and stroke. Cerebral Palsy affects two million children and adults in the United States, with an additional 10,000 babies and infants diagnosed with the condition annually. There is currently no cure for cerebral palsy and no standard therapy.
Hypoxia / Anoxia
Many different phrases are used to describe insults to the brain that result in lack of oxygen or blood flow to the brain, both of which may produce brain injury. A relative lack of oxygen is known as hypoxia, whereas an absolute lack or deprivation of oxygen is known as anoxia. A lack of blood flow to the brain is termed ischemic insult. There are various scenarios that may lead to hypoxic ischemic brain insults. These include drowning, heart attacks, intra-operative complications leading to cardiopulmonary arrests, respiratory arrests, carbon monoxide poisoning, and other toxic exposures.
Various classifications for these types of injuries have divided hypoxic/anoxic injuries into four categories:
- anoxic anoxia – due to inadequate oxygen supply
- anemic anoxia – due to inadequate oxygen carrying capacity of the blood
- stagnant hypoxia – due to the critical reduction of cerebral blood flow or pressure
- toxic anoxia – due to toxins or metabolites that may interfere with oxygen utilization
Incidence of TBI
Traumatic brain injury (TBI) is the leading cause of disability and death in children and adolescents in the U.S. The Centers for Disease Control and Prevention, reports that the two age groups at greatest risk for TBI are aged 0-4 and 15-19.
Among those aged 0 to 19, each year an average of:
- 62,000 children sustain brain injuries requiring hospitalization because of motor vehicle crashes, falls, sports injuries, physical abuse and other causes
- 564,000 children are seen in hospital emergency departments for TBI and released.
Among children aged 0 to 14 years, TBI results in an estimated:
- 2,685 deaths
- 37,000 hospitalizations
- 435,000 emergency department visits
In its 2004 Report to Congress, Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths, the Centers for Disease Control and Prevention notes falls are the leading cause of TBI for children aged 0-4.
Approximately 1,300 U.S. children experience severe or fatal brain trauma from child abuse every year.
Symptoms
| Physical Impairments | Cognitive Impairments | Emotional Impairments |
|---|---|---|
| speech | short term memory deficits | mood swings |
| vision | impaired concentration | denial |
| hearing | slowness of thinking | self-centeredness |
| headaches | limited attention span | anxiety |
| motor coordination | impairments of perception | depression |
| spasticity of muscles | communication skills | lowered self-esteem |
| paresis or paralysis | planning | sexual dysfunction |
| seizure disorders | writing | restlessness |
| balance | reading | lack of motivation |
| fatigue | judgment | difficulty controlling emotions |
Any or all the above impairments may occur to different degrees. The nature of the injury and its consequences can range from mild to severe, and the course of recovery is very difficult to predict for any given child. With early diagnosis and ongoing therapeutic intervention, the severity of these symptoms may decrease in varying degrees. Symptoms can differ greatly depending on the extent and location of the brain injury. Impairments in one or more areas (such as cognitive functioning, physical abilities, communication, or social/behavioral disruption) are common.
Recovery
What makes a brain injury in children different from that of adults?
While the symptoms of a brain injury in children are like the symptoms experienced by adults, the functional impact can be very different. Children are not little adults. The brain of a child is continuing to develop. The assumption used to be that a child with a brain injury would recover better than an adult because there was more “plasticity” in a younger brain. More recent research has shown that this is not the case. A brain injury has a more devastating impact on a child than an injury of the same severity has on a mature adult. The cognitive impairments of children may not be immediately obvious after the injury but may become apparent as the child gets older and faces increased cognitive and social expectations for new learning and more complex, socially appropriate behavior. These delayed effects can create lifetime challenges for living and learning for children, their families, schools and communities. Some children may have lifelong physical challenges. However, the greatest challenges many children with brain injury face are changes in their abilities to think and learn and to develop socially appropriate behaviors.
Common deficits after brain injury include difficulty in processing information, impaired judgment and reasoning. When an adult is injured, these deficits can become apparent in the months following the injury. For a child, it may be years before the deficits from the injury become apparent.
Concussion in Children
Concussion in children is common. Parents often ask, “When it is safe for a child to return to play or other activities?” and “How can I help my child recover from a concussion?”
Infants, Toddlers and Preschool Children
Very young children (i.e. infants, toddlers, and preschoolers) frequently sustain bumps and bruises to their heads from a host of mechanisms including falls (down stairs or from heights such as counter tops or beds), direct impacts (e.g. getting hit in the head with a ball), motor vehicle crashes, tricycle/bike accidents or child abuse.
Sometimes these events can be significant enough to result in a concussion. Deciding whether a child who has hit his head needs an immediate concussion assessment can be difficult. Young children may have the same concussion symptoms as older children, but they do not express them in the same way. For example, young children cannot explain a feeling of nausea or amnesia or even describe where they hurt. Parents and physicians should keep this in mind when considering the presence of concussion symptoms listed below. When in doubt, refer a child for immediate evaluation. Primary care physicians (PCPs) should ask caregivers about all “bumps on the head” and should consider referring a child with a “bump on the head” to the emergency department if they suspect a concussion.
Acute signs and symptoms of a concussion:
- Vomiting
- Headache
- Crying and inability to be consoled
- Restlessness or irritability
Follow-up in Young Children who have Sustained Concussions
All children with concussion or suspected concussion should be followed closely by their PCP. A follow-up visit with the PCP after the event can offer the opportunity for families to ask questions and for the PCP to assess the child for ongoing symptoms. Although diagnosing post-concussion syndrome in young children is difficult, it is important to assess for these symptoms to determine if further evaluation is needed. The follow-up visit can also provide an important opportunity for discussion of age-appropriate injury prevention to minimize the possibility of subsequent concussions.
Infants and young children less than 3 years of age who have had a concussion can have their development tracked by their county’s developmental program for young children. This is particularly important for children who have sustained a complicated concussion (i.e., a concussion with contusions or hemorrhage apparent on imaging), those who have had multiple concussions and/or those with underlying neurologic disease.
Persistent signs and symptoms to assess for during follow-up:
- Excessive crying
- Persistent headache
- Poor attention
- Change in sleep patterns
- Seizures
- Dizziness or confusion
- Change in personality
- Change in nursing or eating habits
- Becoming upset easily or increased temper tantrums
- Sad or lethargic mood
- Lack of interest in favorite toys
Children who display these symptoms for more than several weeks after a concussion may require further assessment and/or evaluation by a neuropsychologist, neurologist, or another specialist.
Child Abuse
Young children may also sustain mild to severe TBIs from abuse.
- Approximately 1,400 cases of abusive TBI (including concussions) occur in the U.S. each year.
- Injuries resulting from abusive TBI and other types of child maltreatment are often unrecognized or underreported.
- Recognition of abusive TBI in young children is critical. If children are returned to a violent home, they are at very high risk of being hurt again or killed.
- In any young child with injury to the head, it is imperative to assess whether the history provided for the injury is developmentally appropriate for a child that age. If not, it is important to consider child abuse in the differential diagnosis.
- In some cases of abuse, caretakers do not report a history of any trauma either because (a) they do not know that there has been trauma because it is being inflicted by someone else without their knowledge or (b) because they don’t want to tell. Thus, if an infant or young child presents with the signs and symptoms listed above, it is important to consider the possibility of abusive TBI even in the absence of a history of trauma.
References: Sources:
Langlois JA, Rutland-Brown W, Thomas KE. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2004.
Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF. A population-based comparison of clinical and outcome characteristics of young children with serious inflicted and noninflicted traumatic brain injury. Pediatrics. 2004 Sep;114(3):633-9.
Shaken Baby Alliance Fact Sheet, Centers for Disease Control and Prevention’s Toolkit for Physicians and the Brain Injury Association of America http://www.biausa.org/index.htm